About IRM
Institute of Reproductive Medicine

A brainchild of Late Prof. Dr. B.N. Chakravarty, IRM was established in 1987 at Salt Lake- DD Block to complete the unfinished work of Late Dr. Subhas Mukherjee, after his unfortunate demise, who pioneered the delivery of “First Test Tube Baby” in India and the 2nd in the world.
Late Prof. Dr. B.N. Chakravarty trained a team of dedicated young doctors, who with their sincerity, devotion, and knowledge, helped infertile couples at IRM to fulfil their dreams under his guidance. This culminated in the delivery of the 3rd Test Tube Baby in November 1986, marking a significant milestone in Late Prof. Dr. B.N. Chakravarty’s clinical career.
Due to a lack of space at IRM Salt Lake – DD Block and increasing numbers of infertile couples, Late Prof. Dr. B.N. Chakravarty set up a second building at Salt Lake -HB Block. Approximately 3,000 to 3,500 new patients visit every year, and 20 to 30 doctors enrol in the training program annually. To date, about 7,000 babies have been born through IVF.
Institute is registered under Societies Registration Act, 1961
Our Services
We offer the following treatments:
Ovulation Induction
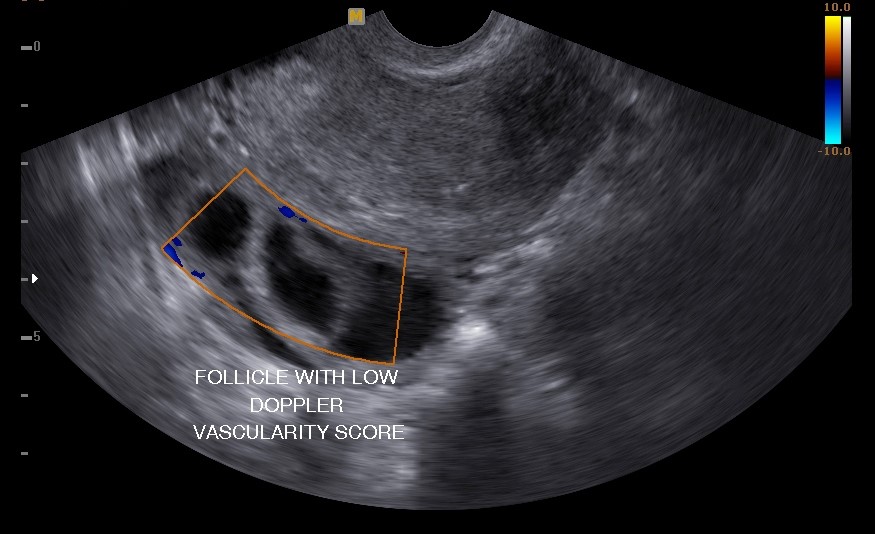
By different drugs, more than one follicle are recruited in the ovaries to increase the chances of conception.
.jpg)
In-vitro Fertilization (IVF)
It is a process by which gametes from both partners are collected and fertilized outside the body within a laboratory atmosphere closely resembling the mother’s womb. The resultant embryos are transferred into the uterine cavity.
Oocyte retrieval: After super ovulation, female gametes (oocytes) are collected under G/A through USG guidance within 34.5 to 36 hours of ovulation induction.
Insemination: Mixing of both gametes in a certain proportion (1 oocyte/30000 motile sperms) is done within 4 to 6 hours of oocyte retrieval, followed by sperm preparation from husband’s or donor’s semen sample.
Embryo culture: Fertilized oocytes or zygotes are cultured in media within a CO2 incubator until day 3/day 4 embryo or blastocyst development. Two good-quality embryos or one good-quality blastocyst are replaced into the mother’s womb by a technique known as embryo transfer.
Embryo transfer: Usually, two day 3 or day 4 good-quality embryos or one day 5 embryo (blastocyst) are loaded in 40 μl media in a catheter and introduced into the uterine cavity under USG guidance for implantation.
Intra-uterine insemination (IUI) using husband's sperm
After ovulation, confirmed by USG, post-wash motile sperm solution (> 3 mill/ml), prepared from husband’s semen, is introduced into the uterine cavity by a catheter.
Intra-uterine insemination (IUI) using donor sperm
By different drugs, more than one follicle is recruited in the ovaries to increase the chances of conception.

Intra-cytoplasmic sperm injection (ICSI)
It involves the injection of one live sperm into the cytoplasm of a metaphase II oocyte in cases of severe male factor infertility or azoospermia.

Oocyte / Embryo freezing
Oocyte freezing is done for donor oocyte banks and when male gametes are not available for insemination on the day of ovum pick-up. Embryo freezing is done for frozen embryo transfer and surplus embryos following embryo transfer in a fresh IVF cycle.

Sperm freezing
Sperm freezing is done when male partners are unavailable on the day of insemination or unable to produce semen on demand. It is also used for fertility preservation before chemotherapy or radiotherapy.

Surgical sperm recovery
In cases of azoospermia where sperms are not available in the ejaculate, sperms are retrieved from the testis or epididymis using techniques like PESA, TESA, or TESE. Sometimes sperms are retrieved through open biopsy or microsurgery.

Egg Donation
Donated oocytes from eligible women are used for conception in cases like premature ovarian failure, surgical removal of ovaries, or age-related decline in fertility in women under 50 years.
Surrogacy
Women unable to carry their own child due to uterine issues can opt for surrogacy as per the ART Bill June 2022.
Stem cell infusion / Mononuclear cell infusion
Used for women with repeated unsatisfactory endometrium in IVF cycles. Mononuclear cells from the woman’s peripheral blood are isolated and infused into her uterine cavity to promote implantation.
Male Infertility
Male factor infertility is rising, contributing to 50% of infertility cases. Causes include environmental pollution, lifestyle changes, and prolonged exposure to electromagnetic fields. Evaluation of male infertility involves a combination of tests.Male factor infertility is rising, contributing to 50% of infertility cases. Causes include environmental pollution, lifestyle changes, and prolonged exposure to electromagnetic fields. Evaluation of male infertility involves a combination of tests.
Mild to moderate male factor infertility can be treated by IUI and IVF procedures. Severe cases can only achieve fertilization and conception through advanced techniques.
Services for diagnosing and treating infertile males are provided by experienced doctors and technicians at IRM.
In-house Services:
- Blood and Hormone Laboratory
- Pharmacy
- Ultrasound Unit
- Echocardiogram
Institute of Reproductive Medicine





